EVAPORATE: Icosapent Ethyl on Progression of Coronary Atherosclerosis in
Patients With Elevated Triglycerides on Statin
1.Age ≥45 years with atherosclerosis with at least one stenosis of 20%.
2.
Fasting TG levels ≥150 mg/dL and <500 mg/dL.
3.LDL-C >40 mg/dLand ≤100 mg/dL and on
stable statin therapy (±ezetimibe)
View attachment 334120
It's hard to say if there's any benefits for someone with low fasting triglycerides or not on a Statin. Statin does cause regression and has more pronounced effects at lower LDL levels. Until we get monotherapy results, we cannot confidently say that these effects can be achieved, without statin use.
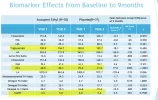
I wonder if the same effect can be achieved by simply bumping up the EPA using otc supplements. Thats a 4x increase in 9 months. 20->89
Either way, i got it ordered and it'll be covered by my insurance if i manage to get it renewed lol
I'm not sure who it was with, but I covered the statin / regression issue regarding the Repatha regression trials, Those subjects were all on statins too.
You can't identify patients with plaque, and take them off their existing statin treatment and pass an ethics review, nor can you find subjects with existing plaque, and not put them on the guideline therapy of a statin to see the results of an experiment. It's considered reckless.
However, it's well established that regression is first and foremost a function of LDL reduction, regardless of the source of that reduction. In EVAPORATE, every type of statin was used, with and without ezetimebe, and the amount of regression, like every other study primarily tracked LDL levels.
What we do know is that statins on their own don't show any fibrous plaque removal. It's essentially immobile without isocapent.
That's huge for maximizing regression.
The other thing we know is calcification slows and essentially stops further regression. So avoiding anything that speeds that process (statins except Pitavastatin, which counters it) should allow it to continue longer for deeper regression.
K2 may help by redirecting calcium away from arteries to bones.
Isocapent lowers inflammation significantly, so I think it can reasonably expected to slow calcification as well, given inflammation speeds it up.
Finally since it's HDL that actually transports the fats being removed from plaque, maximizing HDL quantity AND function (how powerful the "fat vacuums" are, measured by a metric called efflux) will contribute to the speed of regression. Pita preserves and increases HDL numbers, but also improves its function (efflux) considerably.
Below 40 LDL, HDL and efflux become the primary drivers of increased regression.
--------
A funny note:
I removed coconut milk from my diet, because it spiked my LDL. It's also the most potent dietary booster of high quality HDL(it increases efflux not just quantity), vs low quality HDL like niacin. But on balance, it does more harm than good because of the huge LDL boost.
Repatha, Eze, Pita, suppress the LDL increase of 200ml / day of coconut milk, with the net effect being an increase in HDL and efflux that should boost potential regression by ~1.5-2.5% / year, far outweighing any negative impact of the suppressed LDL increase expected to be 0-10 points, clinically insignificant when we're talking about LDL below 40.
On just Pita, Eze 100ml of coconut milk maximizes HDL benefit before LDL outweighs it. Add Isocapent and that rises to 150ml..
I'm going to get a new lipid baseline this week and reintroduce coconut milk to see how this plays out in real life.