just some dude
Member
oh shit, another very useful piece of info, thanks!
heart health is no joke
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: This feature may not be available in some browsers.
oh shit, another very useful piece of info, thanks!
Unless u show uve had a clot on a statin as i did.. then repatha is handed to u and thru insurance is cheap af…Go for Repatha. Keep Pitavastatin in your back pocket for now. Most of the time you're required to "fail" two statins, as well as ezetimebe before Repatha is authorized. I assume you told your doc rosuvastatin was intolerable. Tell them you understand how crucial it is to lower your LDL and would like to try Repatha, but believe you have to try at least two statins first. Let him prescribe whatever, After a week or two call and report the second one is causing intolerable symptoms as well, If they make you try ezetimebe on its own, and then have your lipids checked, stop taking it 10 days before the test, You need to prove it's insufficient to bring your numbers into the guideline range (it probobly is, but you want to ensure that). After this you should be able to get Repatha.
Once the Repatha is prescribed, you're all set. Take it with ezetimebe and start pressing for Pitavastatin. One good argument is that it has a neutral or positive effect on a1c. A completely "diabetic safe" statin.
This triple combo will completely halt progression of plaque, and start to reverse it. Especially as a diabetic, if it remains high after starting Pita, lowering HS-CRP will be the next major risk factor to tackle, to prevent inflammation induced "pimples" from forming within the plaque that can destabilize it and cause
pieces to break off.
Unless u show uve had a clot on a statin as i did.. then repatha is handed to u and thru insurance is cheap af…

Yay for the insurance companies… again… not for those who actually get a stroke or heart attack while on their drugs…I mean basically what we're trying to accomplish here is "trick" the system into giving us the same level of protection they'd normally reserve until AFTER you survive a heart attack or stroke, lol.
If the meds were free, cost effectiveness and "resource conservation" no longer factors, the guidelines would have everyone with >130 LDL on PCSK9 / Statin / Ezetimibe triple therapy.
Funny story, if insurance companies agreed to loosen the preauthorization requirements to cover Repatha, Amgen offered them a a money back guarantee. If someone on Repatha for at least six months has a stroke or heart attack, insurance companies get a full refund for Repatha's cost

Amgen Offers Cholesterol Drug With First Refund Guarantee For Heart Attack Or Stroke Sufferers
Amid concerns about the cost of the drug Repatha, pharmaceutical company Amgen is pledging money back guarantees, making its first such deal with Harvard Pilgrim Health Care. "We want to stand behind the value of our products. We want to put skin in the game," said one of Amgen's senior officials.www.wbur.org
Yay for the insurance companies… again… not for those who actually get a stroke or heart attack while on their drugs…
I mean ive had “high” cholesterol for 20 yrs… and yea it could happen and pray to GOD it doesnt but thats why im going to start ezeti and then work my way up to taking the repatha and the others…
I'm also someone who's had decades of exposure to high LDL trying to stop, reverse, and stabilize risk.
Based on what I know, it may be helpful to think of it like this:
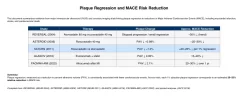
1. LDL below 60 - Plaque accumulation stops.
2. LDL below 50 - Soft plaques regress. First, "fresh" plaque is removed, widening the space within the blood vessel. Then "fatty" content in the old, somewhat stiffened plaque mass is sucked out, leaving "dry" plaque behind. This stops the plaque from being metabolically active, so it's no longer a source of inflammation. (old soft plaque is rotting, the "necrotic core" of the plaque body, pumping out inflammatory particles) After stopping plaque accumulation, inflammation reduction within the arteries is the most crucial factor for reducing long term risk. Inflammation within the plaque causes "pimples" to form between the arterial wall and the plaque, which can cause a piece of plaque to break off, leaving a wound (like a scab getting ripped off), then clotting factors come into heal it, blocking off blood flow, causing a heart attack or stroke.
3. As cholesterol is removed from the plaque, what's left behind is a tough layer (the "plaque cap") that's resistant to breaking up. Eventually it calcifies. Your CAC score will go up, but that's a good thing. Calcified plaque is the most stable form, and as long as you're not laying down any new plaque, you've reached the end stage where risk has been reduced to the maximum possible degree.
All credit to you brother for sparking my interest in finally dealing with my long neglected lipids!
Good to know! Cac is darn near 0… so that may scare people a bit to see it go up… but as long as nothing breaks off to cause issues then thats cool
A CAC of 0 is unlikely to go up. It's possible, I suppose, but calcified plaque is an advanced form of ASCVD, as is the type of plaque that would be calcified once stabilized. One would have to get a CT-CAC at exactly the right moment in the development of soft plaque and prior to the develop of calcified plaque.
I'll take the bump in HDL, but the literature that I've seen suggests that with LDL (a rough proxy of ApoB as we all should know) managed, increases in HDL yield no benefit in outcomes.
Plaque calcification typically takes many years, while significant plaque has been found long before any calcification has taken place, even in people in their early 20s. A recent study found people with 0 CAC score and 90%+ blockage! Statins speed up the process of calcification. (this is considered risk reducing because it stabilizes plaque)
understanding regression is still early science
On this, I'm speculating. Based on some of the data I'm looking at 10-15% of folks with a zero CAC might progress to having a postiive number. The rest likely lack the predisposition.
Could be wrong, grain of salt, and all that. No matter, if a statin causes the CAC score to go from zero to non-zero that's still a good thing. One should get a CTA if they're really worried.
I'll say. Most cardiologists lack an entire clue that this work is happening. Something that makes me mad as hell.
The thing to keep in mind is that until PCSK9 inhibitors like Repatha, reaching the very low LDL needed to reverse plaque significantly was impossible for most people. The leading edge cardiology and pharmaceutical company chatter is all about regressing being the next frontier. For now, reducing risk by "locking it in" using a statin to accelerate calcification makes sense with what's commonly available,
That's why I'm trying to delay it with K2/D3.
If I had a heart attack already though, I'd prioritize stabilizing plaque and forget pursuing max regression,
Likewise. Check the form, either MK-4 or MK-7, one of which is more beneficial.
Agreed 100%

